If there’s any chance you might want to have children (or more children!) in the future, it’s important that you talk with your doctor about your fertility preservation options as soon as possible. Your doctor should refer you to a reproductive specialist. If not, ask them for one.
Even without fertility preservation, some women still get pregnant after breast cancer treatment. Your fertility will depend on a lot of factors, like your age and what type of chemotherapy you received.
If you decide to talk to the reproductive specialist, they will likely talk to you about cryopreservation (freezing your eggs) and ovarian suppression (a way to protect your ovaries during treatment). You can learn more about cryopreservation and ovarian suppression in this downloadable guide.
You can also check out Young Survival Coalition—they have a lot of helpful information about fertility and breast cancer.
If you’re facing infertility, you’re not alone. The Broken Brown Egg has resources on infertility and family building specifically for Black women. Fertility Within Reach has a financial support resources list of infertility treatment grants, adoption grants, and more.


Pregnancy is already one of the most transformative times in your life. Facing a breast cancer diagnosis before, during, or after can be incredibly overwhelming and scary. We’re here to honor both the new life you’re nurturing and the one you’re fighting to protect. Your care team is your best resource right now—they’ll help you understand your specific diagnosis and talk through your options. Reach out to us if you need someone to help you process, navigate, or even just listen.
If you are pregnant when you are diagnosed, your treatment options will depend on the stage of the breast cancer and the trimester of the pregnancy. The American Cancer Society has a helpful page dedicated to breast cancer treatment during pregnancy.

If you are going through treatment after the birth of your child, it’s recommended that you stop breastfeeding around surgery, targeted therapy, and/or chemotherapy. Bobbie—an organic formula company founded by moms—supports moms impacted by breast cancer by offering a full year of Bobbie formula.
If you get pregnant after breast cancer treatment, congratulations! We couldn’t be happier for you and for your growing family! The American Cancer Society breaks down common questions and concerns about pregnancy after breast cancer treatment.


Whether you’re parenting through treatment or navigating what being a mother looks like now, we’re there for you. It’s okay if it feels different than you imagined. Even when it feels like an impossible task, your children are lucky to have you as their mom.

Kids often sense when something’s wrong, and sharing about your breast cancer diagnosis in an age-appropriate way can help them feel more secure and less afraid. It’s okay to not have all the answers; what matters most is creating space for their questions, their feelings, and reminding them that they’re loved and not alone.
Knowing and sharing your family health history—your HERstory—can be a powerful tool. It helps you and your loved ones understand your risks, make informed decisions about screening or genetic testing, and take steps toward early detection or prevention. Discovering and sharing your HERstory is a way of caring for yourself and protecting future generations.
Some breast cancer treatments can send your body into temporary or permanent menopause. Early menopause can feel like yet another loss on top of everything else—sudden hot flashes, mood swings, vaginal dryness, and the weight of unexpected change. It’s not just about hormones. Early menopause can affect your sense of identity, your relationships, and your sexuality. You’re not imagining it, and you’re not alone. There are ways to manage symptoms and support your body through it—whether that’s through medication, lifestyle changes, or working with specialists who understand what you’re going through.
Ask your doctor about non-hormonal medications that may help ease the discomfort of your symptoms. Talk to your doctor about vaginal moisturizers and estrogen creams, both of which treat dryness and discomfort. Consider vaginal lubricants for sex–they help prevent irritation and pain during sex by reducing friction. And check out the integrative and holistic care section below!
Breast cancer changes our relationships with our bodies. It can shift your experience of sex, your connection with your partner, and even your preferences—how you like to be touched, what feels good, and what intimacy means to you now.
You’re not alone. All of us have faced difficulties with sex at some point during and after breast cancer treatment.
Adjusting takes time, and that’s okay. You will find what feels good to you now. Sexual wellness isn’t just about the physical—it’s also deeply connected to your emotional health, your sleep, your nutrition, and your overall well-being. A helpful first step is to name what’s going on for you, so you can start to build a plan that supports your needs.
Don’t hesitate to bring up sexual health with your doctor, social worker, or nurse navigator. These conversations can feel vulnerable, but they’re important and your care team is there to help. Be as specific as you can about what you’re experiencing, whether it’s discomfort, pain during sex, or changes in desire. There are specialists who focus on helping people have better sex during and after cancer, like sex therapists, pelvic floor physical therapists, and couples counselors, all dedicated to helping you reconnect with your body and your sexuality.





Whether you’re parenting through treatment or navigating what being a mother looks like now, we’re there for you. It’s okay if it feels different than you imagined. Even when it feels like an impossible task, your children are lucky to have you as their mom.

Navigating a relationship during and after breast cancer is hard work.
Remember: it’s okay to grow and redefine your connection together as often as you need.
Going through a divorce during or after breast cancer adds another layer of grief, another transition to an already tough time. But it can also be a turning point—a chance to reclaim your sense of self, rebuild on your own terms, and choose what healing looks like for you.


Balancing school or a career while going through breast cancer can feel overwhelming—you’re juggling deadlines, expectations, and very real side effects. It’s okay to set boundaries, ask for accommodations, or take a step back when you need to. You’re not falling behind—you’re surviving, adapting, and showing up in ways that take real strength. Give yourself permission to redefine success on your own terms.



It doesn’t matter if you’re a first year college student or a new hire—you have the right to speak up for yourself.
Talk to your dean or your Human Resources department. They can help you to understand your options around medical leave, disability services, flexibility and accommodations around deadlines and attendance, and more. If you are self-employed, you should go to your state’s HR Department online for resources.
Your family, friends, and advocacy groups like TOUCH want to support you. Reach out for help. No one should face breast cancer alone.
After breast cancer, your body might feel unfamiliar. You might even feel betrayed by your body. We’ve been there. But embracing body positivity doesn’t mean pretending everything is perfect; it’s about recognizing your strength, honoring what your body has been through, and finding ways to celebrate it just as it is right now. Your body is resilient. Your body has the capacity to heal.
Watch Dr. Monique Gary talk about navigating body image challenges and cancer at a Unite for HER virtual hangout.



Depending on your treatment, you might experience side effects that can impact how you look. While your doctor may talk to you about some of these side effects—like hair loss from certain chemotherapies—they may not know about the side effects that are specific to Black women. For instance, many Black women experience extremely dry skin and/or darkening of their nails over the course of treatment. Products like Nerak cream and Marquita GoodLuck Radiation Butter–even on your nails–can help!
Breast Cancer Prevention Partners’ Black Beauty Project hosts an incredible database of trustworthy non-toxic Black-owned beauty products and brands.

Integrative & holistic care are both terms for all of the therapies and modalities that exist outside of conventional medicine, like acupuncture, massage, meditation, nutrition, supplements, yoga, therapy, and healthy lifestyle choices. Adding these interventions into your treatment or survivorship plans can help to reduce stress, manage side effects, make it easier to stay on your treatments, help you sleep, and improve your quality of life.
The National Center for Complementary and Integrative Health has a comprehensive A-Z list of all things integrative health. For every supplement and approach, you can find reliable and trustworthy data about if and how it works.
You can find workout classes at Moving for Life or through the Cancer Exercise App, which helps you to develop a personalized exercise program and track your progress. Exercise is Medicine’s Moving Through Cancer lets you find resources in your community.
Therapy for Black Girls and Black Emotional and Mental Health Collective are both thoughtful resources that house directories of Black therapists.
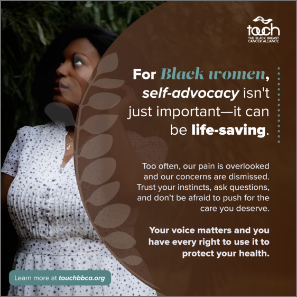
For Black women, self-advocacy isn’t just important—it can be life-saving. Too often, our pain is overlooked and our concerns are dismissed. Trust your instincts, ask questions, and don’t be afraid to push for the care you deserve. Bring someone with you to appointments, take notes, and find providers who listen. Your voice matters and you have every right to use it to protect your health.



When you consider enrolling in a clinical trial, you’re not only investing in the most cutting-edge treatments for yourself, but you also take the first step towards helping to develop better TNBC treatments for all Black women.
You should consider a clinical trial any time you are making a breast cancer treatment decision. There are opportunities for people with all stages and types of breast cancer—from those newly diagnosed to those in treatment to those in remission—to participate in clinical trials. Ask your doctor about clinical trials early and often.